“I Always Wanted to Do It Online”: Systemic Challenges Faced by Immigrant New Yorkers When Renewing Their Medicaid
Systemic barriers such as long wait times, technology limitations, and Medicaid offices that are difficult to reach make enrolling in Medicaid challenging for far too many New Yorkers.
From the IRI survey and interviews, we have found that immigrant New Yorkers experience various challenges when renewing their Medicaid that make an already long and difficult process more time-consuming and challenging. Survey respondents and interviewees expressed difficulties that fall into three main types of challenges: language access, physical inaccessibility and technology access.
Language Access
In 2022, New York State codified and expanded language access laws throughout the state, which requires that all state agencies, that interact with the public, offer translation services to those who need it, and translate vital documents into the top 12 most commonly spoken languages. Our survey and interviews with immigrant New Yorkers revealed that New York State is doing well on making Medicaid forms accessible in multiple languages, but not as good at providing interpretation services. Translation is when documents are converted from English to a different language, but interpretation includes in-person and over the phone simultaneous oral explanation and American Sign Language interpretation. The overwhelming majority, 93 percent, of survey respondents were able to access the Medicaid forms in a language that they could understand. This is a great testament to the work that New York State has done, however, there is still much further to go to ensuring that everyone, regardless if English is their primary language or not, can access critical public services.
The Overwhelming Majority of Survey Respondents Were Able to Access the Medicaid Forms in a Language That They Could Comfortably Read and Write
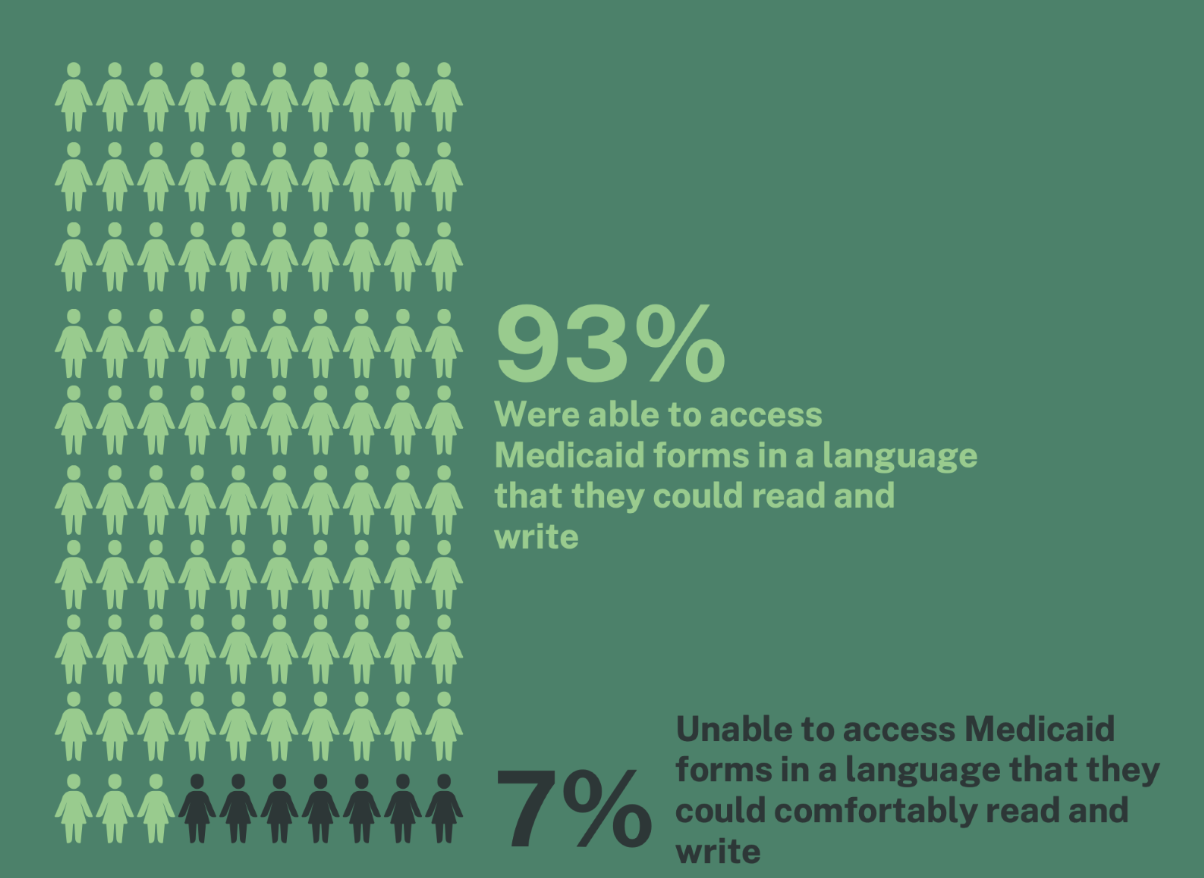
Fig 1. Immigration Research Initiative Survey
The majority of survey respondents who needed an interpreter were offered one, which is a positive sign. But a substantial portion, 39 percent, of those who needed an interpreter did not get one. Although respondents felt like New York State did a good job providing documents that were translated in the languages that were needed, a survey respondent recommended that “friendly translators” (by which respondents mean interpreters who translate in real time) would make a profound difference in the experiences of immigrants who rely on these personal oral explanations.
The Majority of Respondents Who Needed an Interpreter Were Offered One
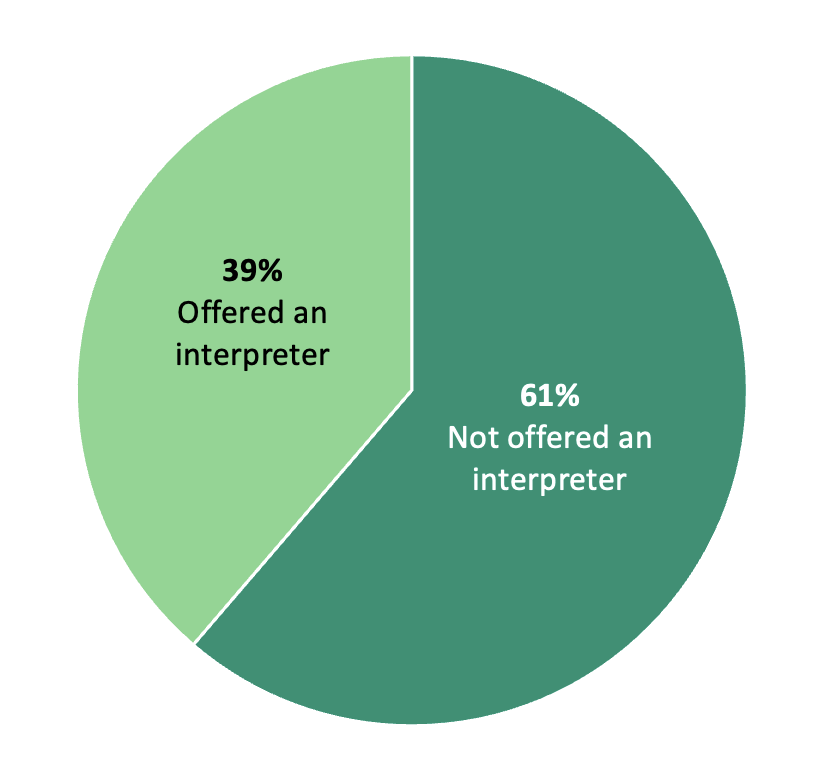
Fig 2. Immigration Research Initiative Survey
New York State has enacted the Translation Services Law, but this survey highlights that there are still people who are being left out and struggle to access information because of language barriers. Nearly 40 percent of respondents who needed an interpreter were not offered one. This surfaced in our interviews where one respondent shared that the most difficult part of enrolling in Medicaid was that there was “no one to translate” highlighting the need for interpreters who can help in real time with oral translation. Another survey respondent shared that access to a “language interpreter” would have made the renewal process easier.
Language access is very important in a state like New York with a large immigrant population and 800 languages spoken by residents. Many respondents shared stories of relying on friends and family to help them overcome the language barriers that they faced when tasked with enrolling or renewing their Medicaid. One interviewee highlighted the importance of family and friends in helping with successful Medicaid renewal: “Sometimes we need help going through the forms. Even though we can read English, we might not be able to understand some of the legal terms. I was actually fortunate enough to have a cousin there with me to explain some of the words in the terms for me.” The reliance on friends and family to overcome these systemic issues, that should be able to be addressed by the government whether or not people have access to family assistance, is something that came up throughout our analysis.
In 2020, when the global COVID-19 pandemic caused an increased demand for public health benefits, the federal government made it possible for people who were already enrolled in Medicaid to be automatically re-enrolled. This automatic re-enrollment ended in 2023 a policy commonly called the unwinding of Medicaid continuous enrollment.
Of the many methods of communication that New York State used to notify consumers to re-enroll in Medicaid, one was mailed notices. Of the people who we surveyed, 15 percent never received a notice in the mail. Of the respondents who received a mailed notice, 11 percent did not understand it and 27 percent needed help from someone else to understand it. Although most of our respondents were able to understand the notices that were sent (62 percent), the stories from the other 38 percent of immigrant New Yorkers are still important and deserve to be heard in order to make this program better and to improve future communications and outreach efforts.
Most Respondents Understood the Notices That They Received in the Mail However Many Did Not or Needed Help Understanding
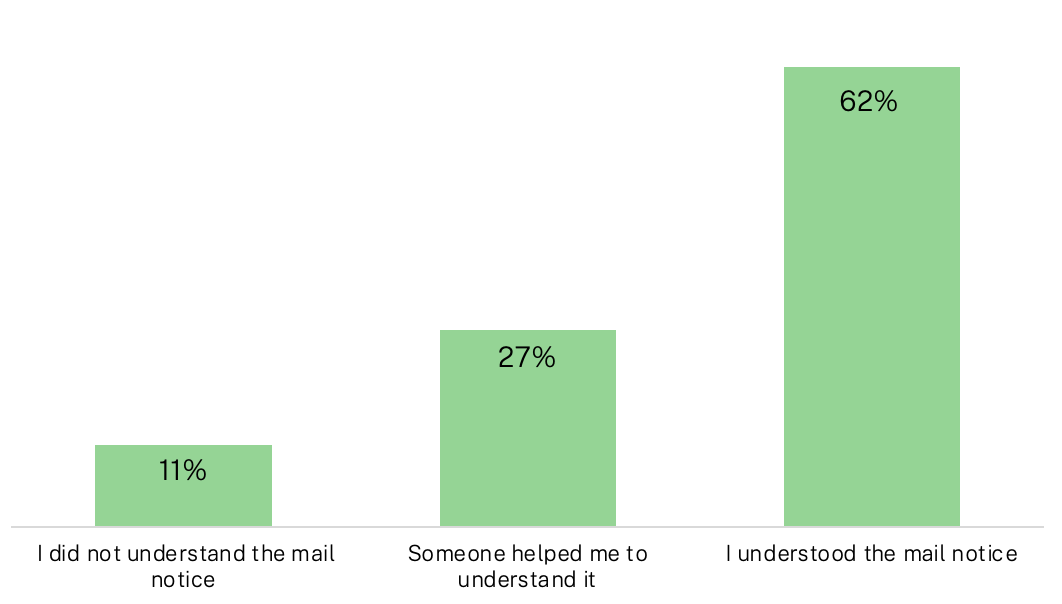
Fig 3. Immigration Research Initiative Survey
The “language barrier” experienced by many of our participants while enrolling or renewing their Medicaid was also present as they received communications from the Medicaid office. Perhaps the notices were not in their native languages or maybe they struggled with the words that were used, which was a common complaint. Nearly 30 percent of our respondents needed help from other people to understand the mailed notices from Medicaid, which signals a problem with this method of communication. One respondent shared their twofold struggle, not understanding the Medicaid forms and not receiving notices: “Challenges in understanding the language and big words leading me to input inaccurate details, and the lack of notices.” The State of New York should do more to ensure that when important notices are being shared, that language access is not an issue and that people are able to receive the support that they need to understand the information being shared.
For the immigrant New Yorkers that responded to our survey, difficulty understanding the critical information on notices and forms was a common theme that made receiving reminders and enrolling/re-enrolling in Medicaid very difficult. This was highlighted by a respondent who wrote that they had an “inability to initially understand the confusing jargons, and there were too many words involved…” When asked about the hardest part of the process, survey respondents and interviewees shared that there was a “Lack of clarity on renewal notice[s].” The U.S. public health care system is notoriously confusing and many of our survey participants shared that this added to the difficulty of enrolling in Medicaid. Vital information is not being conveyed because of language access as a respondent noted that the most difficult part of the process was “reading new guidelines.”
When asked about one thing they would change to make it easier for others survey respondents shared using, “clear and concise text” and “the language and the vocabulary that people have to go through.” In fact, respondents felt that removing “…unnecessary language where possible…” and eliminating “the usage of confusing words” would help them in their pursuit to enroll in Medicaid by making forms and other methods of communication easier to understand.
Throughout our interviews of immigrant New Yorkers who were enrolling in or renewing their Medicaid we heard similar testimonies of struggling to overcome the language barriers that are present throughout the entire process of securing Medicaid as a health insurance provider. In some interviews we heard feedback that would specifically help address how to make the process better for immigrants. To overcome the language barrier some suggested that Medicaid use simpler language: “So, basically when you are sending out forms, it always good to use the general language—basic words and language that everyone can easily understand.” Another participant shared similar advice noting that because the language used is difficult to understand they have to rely on other people which makes an already difficult process harder: “I would say it would’ve been pretty easy for one thing if they use simpler words to describe what I needed to do because some of the terms they were using were really difficult to understand. It’s like I needed someone to complete every sentence because it’s stressful, you know… So, it’s really, really challenging for me.”
Language access is a systemic issue that must be addressed to help support immigrants enroll in and stay enrolled in Medicaid. It is a critical issue that would improve their health outcomes and experiences. We should note that our survey was offered in English, French, and Spanish, and interviewees were offered to speak with an interpreter for the interview portion.
Technology Access
Throughout many survey responses and interviews, participants shared that submitting their documents or completing their application was made more difficult because they lacked the technology needed to do so. There are multiple pieces of technology required to submit an application online: access to computers, scanners, and high-speed internet and sometimes more. For immigrants who are applying for Medicaid, these tools are not always readily accessible and can be expensive or hard to come by. In an interview we heard a story about someone who tried to complete their application online but couldn’t: “I can still remember about the enrollment process. I felt it was a little bit difficult because of the sheer amount of time-consuming questions that were in the document and typing in the application. I lacked the necessary hardware for me to make it online.”
For many of the immigrants surveyed, “technical difficulty,” was a recurring theme in the challenges to enrollment that they faced. After trying to use their own computer one interviewee shared that they ended up visiting a Medicaid office for help: “Yeah, at first technology failed me, so I had to go to the offices.” Some encountered setbacks with “network traffic” and “network issues” which highlights that having stable internet access is a major part of the lack of technology.
Even if respondents had access to computers and internet, the actual process of uploading and submitting files was difficult as some described the “technical difficulty” and “technology advancement” of the enrollment process. Enrolling in Medicaid requires consumers to provide many sensitive documents to prove and verify identity and determine eligibility. Experiencing technical difficulties when sharing sensitive data is a risk to immigrant New Yorkers. This task is not easy for many, as a respondent noted when sharing about using the online service that they encountered “problems proving identity remotely.” Another respondent wanted to use the online system but couldn’t, sharing in an interview, “I can still remember that I clearly had issues with technology. I always wanted to do it online.” We also heard a story about someone who wanted to submit their application online but couldn’t because they didn’t have their own computer. Here’s how they described their feelings about not having the necessary technology: “It was definitely a letdown.”
Technology access is a systemic issue that impacts immigrants applying for Medicaid. These challenges can be difficult, and expensive, to overcome. New York State should reduce network issues to ensure the safety of enrollee’s personal information.
Medicaid Office Visits
Visiting a Medicaid office for help is an option that is available to everyone however, we identified challenges that many immigrant New Yorkers face when seeking assistance in-person. Recurring themes that our respondents shared in their stories were inaccessible locations, long in-person wait times, and not finding the service helpful. These systemic issues make applying for or renewing Medicaid more difficult, risking vital access to healthcare that immigrants, and other New Yorkers need.
For some, taking time off work can be challenging. An added difficulty is that with visiting the Medicaid office in-person, wait times are long, and sometimes it takes more than one visit to finish an application or resolve an issue or question. For the immigrant New Yorkers that we surveyed, these experiences were very common. A participant shared that it was hard to take time off from work. For this person, “unpredictable work schedules” are what made the process more difficult. When asked about if they ever had an in-person visit at the Medicaid office one respondent shared, “I actually had to leave my workplace in order to do that. I actually had to ask permission to be absent on the day so that I can do that. So I stayed away from work because of that. And although there were just no serious implications, because I work in a store, it was just time that I took off work.” For some immigrant New Yorkers, taking time off, sometimes more than once, can be a heavy burden.
Another theme that was identified was difficulty getting to Medicaid offices due to inaccessible locations. Many of the immigrant New Yorkers that we surveyed shared that traveling long distances was challenging. One survey respondent made sure to emphasize that “taking time off work to travel LONG distances for the renewal process” was hardest part of the process. In an interview, we heard a story of someone who drove 45 minutes to get to a Medicaid office and then waited three hours to be seen. The chief complaint wasn’t the wait time, because they needed the help, it was that they couldn’t go back to the office because it was so far away from where they lived: “So it [the Medicaid office] wasn’t a close place to my area. So that was like the main reason I couldn’t go back there because it was actually not very accessible, you know? Time was too much. So I tried online.”
Some participants didn’t find the service helpful even though they visited the Medicaid office in-person. The following respondent felt that their time was wasted by going to the office and not receiving help: “The hardest part for me was the constant procrastination by the Medicaid office…Bringing in unnecessary steps each time I revisit just to screen me out…it was so frustrating.” Another story we heard shows how some people leave or give up when they aren’t able to get help from Medicaid staff, “Yeah, at first I went in person, but I think that did not work for me. So I came back home and I tried it online.”
In one of our interviews a person shared an idea for making office visits easier for people with disabilities: “Special care for the impaired. We should be given priorities like that attention when we visit the offices. We should be given a special treatment, unlike other people. So, priority to us should be given first on that. Another thing is the assessment of all the information. Like whenever you have to renew your [coverage], just one could just apply it online and that determination process could just be granted. So that’s one of the things that I’d really recommend to be implemented and it’ll be of great benefit.”