“I Could Not Understand the Form”: Challenges for Immigrant New Yorkers During the Medicaid Unwinding
Enrolling for or renewing one’s Medicaid can be a challenging and time-consuming process for anyone. It is even more difficult for immigrants who may not speak English and lack knowledge about the healthcare system in the United States. To better understand the challenges immigrants face enrolling and re-enrolling in Medicaid, Immigration Research Initiative (IRI) conducted a survey that garnered 54 responses from immigrant New Yorkers who had gone through the Medicaid enrollment process. We conducted in-depth individual interviews with 20 of the respondents.
The survey took place between June and September 2023, during a period in which many people suddenly had to re-enroll in Medicaid, a period often referred to as the “unwinding period.”
At the beginning of the COVID-19 pandemic, the US government enacted the Families First Coronavirus Response Act (FFCRA), which required that state Medicaid programs keep recipients continuously enrolled until the end of the public health emergency, which meant that recipients did not have to submit renewal paperwork. This research examines the renewal experiences of immigrant New Yorkers during the unwinding period, which is defined as the period after April 1, 2023, the date when Medicaid agencies were required to begin redeterminations for Medicaid enrollment due to the end of the continuous enrollment requirement that was enacted under the FFCRA.
The survey was done through outreach to different communities, and reached a diverse sample but not one that is representative of the overall population of immigrant Medicaid recipients. Of the 54 people who responded to the survey, 70 percent identified as Black/African American, 9 percent as Asian/Pacific Islander, another 9 percent as white, 6 percent as more than one race, 4 percent as Hispanx/Latinx, and 2 percent as American Indian/Alaskan Native. Overall, among both immigrants and non-immigrants living in New York State, 34 percent of Medicaid recipients are white, 30 percent are Hispanic/Latinx, 19 percent are Black, 10 percent are Asian or Pacific Islanders, and 0.2 percent are Native American or Alaskan Natives.
Although this research is a good representation of Black/African American experiences, it is not representative of all racial groups experiences due to low response rates from other racial groups, specifically from Hispanic/Latinx individuals. Outreach attempts were made to try and increase Hispanic/Latinx responses to this research including translation of materials in Spanish and direct outreach to community-based organizations that serve Hispanic/Latinx New Yorkers.
All survey respondents and interviewees were immigrants who live in New York State. Over half (56 percent) of respondents have a green card, almost a quarter (22 percent) have a visa, 15 percent are refugees, and 6 percent chose not to answer.
The goal of this research was to assess the efficiency of outreach practices used by New York State during the unwinding and to better understand the challenges that were prevalent for immigrant New Yorkers when renewing their Medicaid during the unwinding period.
According to the IRI survey, 78 percent of survey respondents felt that the New York State government did a good job conducting outreach to inform individuals about required renewals. The government used numerous methods to inform Medicaid enrollees that they had to renew, including mailed notices, social media posts, text messages, website updates, television ads and more.
Over Three Quarters of Survey Respondents Thought NYS Did a Good Job Conducting Outreach Informing Medicaid Recipients of Required Renewals
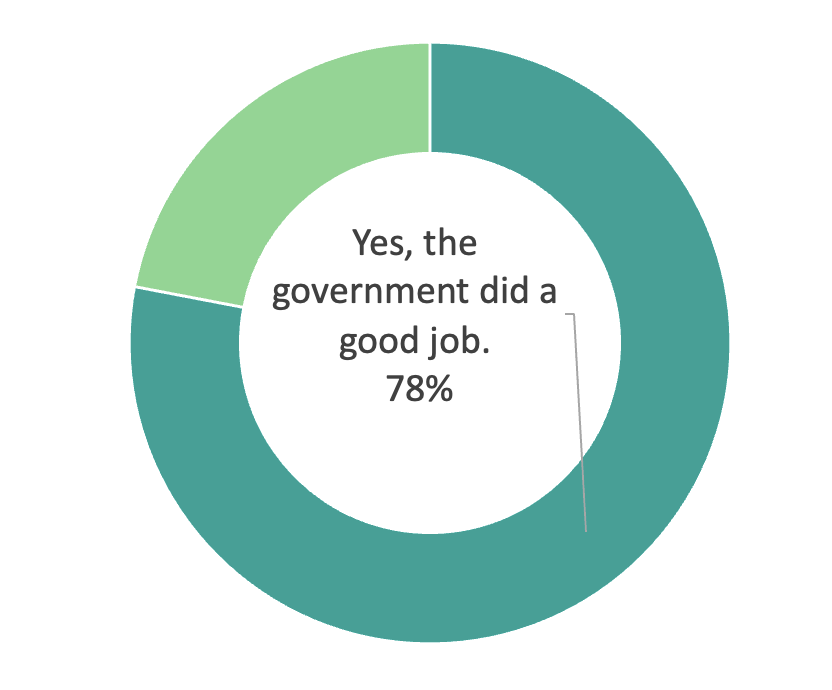
Fig 1. Immigration Research Initiative Survey. Based on 54 responses.
Despite a majority of interviewees and survey respondents feeling that the government did an effective job ensuring everyone knew that they were required to renew their Medicaid, the expression of challenges during the renewal process, including technology difficulties, language access challenges, long wait times and experiences of discrimination from Medicaid personnel, left a majority of respondents feeling that the government could do a better job with the renewal process. Many respondents and interviewees expressed that the challenges experienced during the renewal process made the process confusing, more difficult, longer, and stressful.
The findings from our research highlighting the challenges are outlined in a series of short reports:
- “I Always Wanted to Do It Online”: Systemic Challenges Faced by Immigrant New Yorkers When Renewing Their Medicaid
- “My Papers Were Incomplete and It Kept Being Denied”: Challenges with the Medicaid Renewal Process
- “I Am Transgender, So It’s Obvious Why They Didn’t Want to Attend to Me”: Discriminatory Experiences of Immigrant New Yorkers During Medicaid Renewal
Based on the survey responses and interviews with immigrant New Yorkers who went through the Medicaid renewal process during the unwinding, IRI can summarize the following recommendations for New York State to make the process less challenging and time-consuming:
- Expand support for community-based organizations to assist with Medicaid renewals. 63 percent of survey respondents had help from others filling out their Medicaid renewal application. Trusted organizations often have interpretation services, are knowledgeable about the Medicaid application process and can provide friendly support to individuals who need assistance with the renewal or application process. This ensures that all eligible individuals are able to complete the application and reduce inappropriate Medicaid terminations or denials.
- Ensure that all Medicaid agencies are offering interpretation services, not just translation of documents. 93 percent of survey respondents expressed that they had access to translated forms. Despite good availability of translated documents, some respondents expressed that they were not offered an interpreter, that is to say, a person who can verbally translate and not just translated written documents. There should be an internal review process in place to ensure that Medicaid personnel are offering interpretation services to those who need it.
- Require diversity training for all Medicaid staff. No enrollee should be treated differently or unfairly for the language that they speak, their race or ethnicity, their religion, their gender identity, their disability or any other characteristic by Medicaid staff. Diversity training would help ensure that all staff are culturally competent to interact with a diverse community.
- Develop a clear process for reporting discrimination at Medicaid offices. The Medicaid office should have clearly outlined policies for reporting experiences of discrimination so that corrective action can be taken and further cases of discrimination do not occur.
- Increase Medicaid office staffing levels to reduce wait times. Survey respondents and interviewees waited multiple days to weeks or even months to receive assistance. To avoid terminations of Medicaid coverage for eligible individuals, the Medicaid office should increase their staffing to ensure everyone gets the help they need.
- Ensure that Medicaid offices are in an accessible location to public transportation. Many Medicaid enrollees are low-income individuals who may use public transportation because they do not own a car or have the money to take long taxi or ride-share trips. Medicaid offices should be in locations that are easy to find and are accessible to public transportation like buses and subways.
- Provide phone or virtual technical assistance to help reduce issues with filling out applications online that can increase successful application completion and document verification.
Thank you to our partners that helped us conduct outreach and connect with community members across New York State.
By Cyierra Roldan, Deputy Director and Shamier Settle, Senior Policy Analyst